Macular degeneration affects millions of people around the world. It begins with very small changes in vision and can result in permanent blind spots, especially when left untreated. While its most serious form (“wet” macular degeneration) only occurs in about 10% of patients with the disease, it evolves from the less severe types and can be delayed, prevented, or even reversed if detected early. Here are seven things you need to know.
1. Age, genetics and lifestyle choices can increase your risk
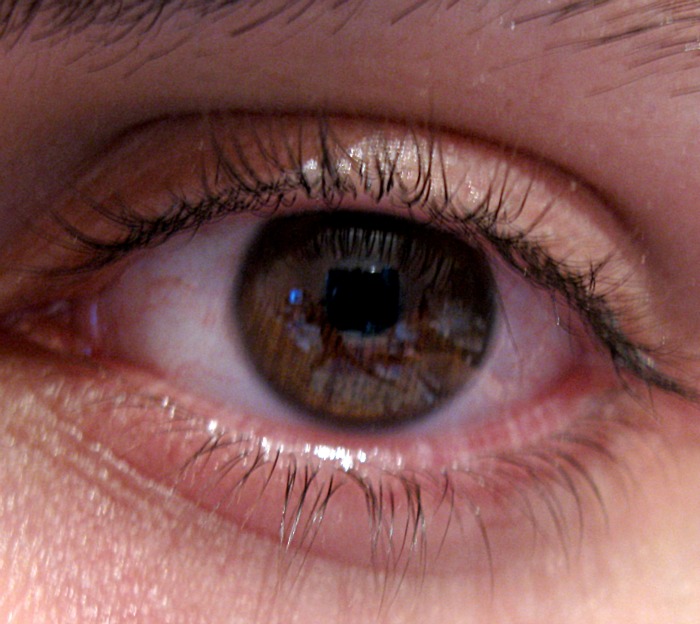
If you’re over 60, a current or former cigarette smoker, or have family members who have been diagnosed, you may be at high risk of developing some form of macular degeneration. Women, people with high blood pressure, Caucasians, and people with light-colored irises may also be more susceptible.
2. Wet macular degeneration is the most serious type of the disease
There are two basic forms of this disease. “Dry” macular degeneration, by the far the more common type affecting as many as 90% of macular degeneration patients, generally causes small changes in vision over a long period of time. As the tissue in the eye slowly breaks down due to the effects of aging, small yellow spots called “drusen” and sometimes blisters may appear. These result in distorted or dark spots in the patient’s field of vision that may not be permanent. This process is sometimes called “geographic atrophy.” Central vision may blur so gradually that it goes unnoticed for months or even years.
General symptoms of macular degeneration include blurred vision, small blind spots, visual distortion (where straight lines and grids may appear wavy), trouble recognizing faces, and difficulty performing tasks that require close examination, such as reading, sewing, and fixing things around the house.
The affected areas may also darken the patient’s vision and make colors seem less intense. Symptoms may appear in both eyes at the same time, or in just one eye. If only one eye presents symptoms, the brain may correct faults in the patient’s field of vision to the extent that no noticeable change in overall vision occurs. However, it is highly likely that the other eye will eventually develop similar symptoms.
Virtually all cases of “wet” macular degeneration develop from the less severe “dry” form, whether or not any symptoms were noticeable. Often as a result of drusen or blisters in the eye tissue and an abnormally high level of “vascular endothelial growth factor” (VEGF), new blood vessels begin to grow beneath the macula. These vessels are unusually fragile.
They often leak and produce swelling and fluid buildup, which can cause scarring of the retina and permanent distortion or loss of vision in the center of the eye. This process is called “choroidal neovascularization” (CNVM). CNVM often occurs suddenly and worsens much more rapidly than other stages of the disease. Visit your ophthalmologist as soon as possible if you experience any sudden blurriness or loss of vision.
3. Being proactive with your eye health can make a difference
Regular exercise, a diet rich in fresh leafy greens and fish, and well-managed blood pressure mean a reduced risk of developing wet macular degeneration, as well as better all around eye health. Remember to protect your eyes from direct sunlight as often as possible with sunglasses that fully cover your field of vision and are rated to block 99 to 100% of UVA and UVB rays.
A vitamin formulation based on a 10-year clinical trial called the Age Related Eye Disease Study (AREDS) recommends a high dose daily regimen of the following vitamins and minerals to protect against and treat macular degeneration: vitamin C, vitamin E, beta-carotene, zinc (zinc oxide) and copper (cupric oxide). The pairing of copper and zinc is particularly important because high doses of zinc supplements taken alone may cause copper deficiency. Because the recommended dosages are much higher than what might typically be recommended to someone not at risk of this or a similar eye disease, patients should discuss the best possible supplement combination with their doctors.
4. Early detection is key
Give your doctor the chance to detect signs of the disease as early as possible. Today there are a number of treatments and therapies that can prevent, delay, and sometimes even reverse the acceleration of macular degeneration. Because the more severe wet form appears and worsens so quickly, an early diagnosis can make a huge difference in preserving a patient’s quality of life. Experts recommend testing specifically for macular degeneration every two years, in addition to regular yearly eye checkups.
Signs of the early stages of macular degeneration are observable with the regular tests performed during a standard eye examination. Visual acuity tests, like chart reading, check for deterioration in the patient’s field of vision. Abnormalities in the nerves and eye tissue are visible to the eye care professional through dilated pupils.
In the advanced stages, CNVM can be detected with a special, non-invasive photographic test called “fluorescein angiography.” Colored vegetable dye is injected into an arm vein and tracked as it travels through the blood stream and passes through the patient’s eye. A series of photographs of the inside of the eye reveal the condition of the eye’s blood vessels and whether or not there are any leakage areas, lesions, or abnormally formed vessels present.
5. There are many new treatment options available
Depending on the type and progression of the individual case, there are more treatment options available today than ever before.
Monthly eye injections may subdue the extra VEGF that wet macular degeneration produces, preventing the growth of new abnormal and misplaced blood vessels. Antibiotic drops may be prescribed along with each shot to reduce the chance of developing an infection at the injection site.
Lasers can be used to prevent CNVM from spreading to the patient’s center of vision. If the disease has already affected the macular center, drugs like Macugen, Lucentis, Eylea and Avastin or a special treatment called “photodynamic therapy” can limit the affected areas of the eye. During a photodynamic therapy session, the drug Verteporfin is injected into an arm vein. It travels throughout the patient’s blood stream and is activated exclusively within the damaged blood vessels of the eye with a special laser.
Once the abnormal vessels are destroyed, the patient’s rate of vision loss is significantly slowed. One therapy session takes about twenty minutes. Full laser surgery is less common when treating macular degeneration, as it may also destroy some of the surrounding healthy tissue in the eye.
Obviously there is acupuncture as well for treating wet macular degeneration. We are having very good success with this treatment.
6. Special resources can help you or a loved one cope with limited vision
A wide variety of low vision devices are available to help people who cope with limited vision due to macular degeneration every day. Large print reading materials and special settings on televisions, phones and computers can help patients continue many of the everyday activities they enjoy. Special devices range from special lighting, magnifiers and high-powered reading lenses to talking watches, clocks, calculators, and telephones, special software and hand-held computers, and scan-to-read devices that can help make everyday tasks both safer and easier at any stage of the disease.
7. You’re not alone
Over 15 million people experience some form of macular degeneration in the United States alone. Between 1.5 and 2 million of those patients are diagnosed with wet macular degeneration. There are specialists, therapists, technicians, clinics and support groups all across the country that are ready to help you and your family deal with the effects of this common eye disease, with the latest information and technology at your disposal.